What is antibiotic resistance?
Antibiotics are medicines used to treat infections that are caused by bacteria. Antibiotic resistance occurs when antibiotics no longer have the ability to effectively inhibit or kill the bacteria. Thus, the bacteria continue to grow and multiply despite the presence of adequate levels of antibiotics in the body.
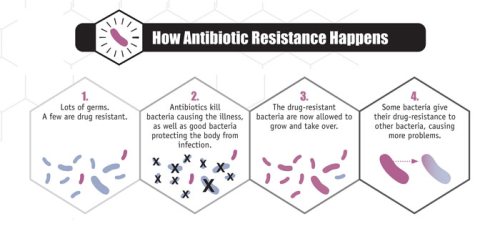
Development of antibiotic resistance among bacteria is a result of ‘survival of the fittest’. Antibiotics will kill or inhibit growth of susceptible bacteria but small number of resistant strains of bacteria will survive and flourish, resulting in development of huge populations of resistant bacteria. This can be a result of overuse and abuse of antibiotics. The situation is made worse as the resistance can be spread to other bacteria.
|
Figure 1. How antibiotic resistance happens |
Why is antibiotic resistance a problem?
Hospital acquired infections are often due to antibiotic resistant superbugs such as methicillin-resistant Staphylococcus aureus (MRSA) or carbapenem-resistant Enterobacteriaceae (CRE). Estimates say that up to 300 million lives will have been lost to infections by drug-resistant bacteria by 2050. If these resistance becomes widespread, antibiotics that are currently effective would no longer work in the future. Without access to effective antibiotics, treatments such as surgery and chemotherapy might no longer be viable because of the increased risk of life-threatening infections after such procedures. Hence, there is a need to act to prevent the rise of antibiotic resistance.
http://www.straitstimes.com/opinion/superbugs-why-they-matter-to-singapore
How do bacteria gain resistance?
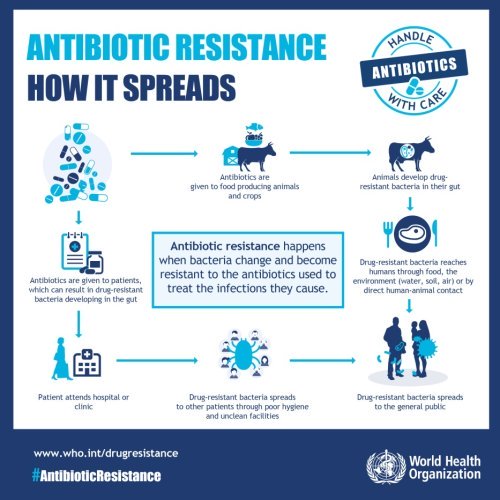
Resistance, like evolution, is a natural process. However, there are other factors can speed up the spread of resistance.
- Exposing bacteria to antibiotics, for example
- Unnecessary use of antibiotics in non-bacterial infections such as in viral infections like the common cold
- Not completing the entire course of antibiotics prescribed
- Use of antibiotics in farming to promote animal growth
- Bacteria spreading its resistance to other bacteria, for example,
- Poor personal hygiene, spreading bacteria with resistance to other people
- Poor infection control in hospital and clinics
- Slow discovery of new antibiotics
How can you prevent resistance?
Use of antibiotics is the biggest contributing factor in bacterial resistance. Here are some tips for you to help prevent resistance,
- Stay healthy! Don’t expose you and your family to antibiotics and hospital environment unnecessarily
- Go for regular vaccinations
- If you are sick,
- Seek help from a doctor, not all sickness requires antibiotics
- Do not share antibiotics
- Make sure you finish the full course of antibiotics even if you feel better
- Practice good personal hygiene, especially hand hygiene! This protects you from getting infection and prevents spreading of bacteria to others too! Wash your Hands, Save your Friends

 Are antibiotics always needed for respiratory tract infections like flu?
Are antibiotics always needed for respiratory tract infections like flu?
Upper respiratory tract infection (URTI) is the most common cause for a doctor’s visit in several developed countries, including Singapore. Signs and symptoms of URTI include: cough, sneezing, runny nose, nasal congestion, fever and a scratchy or sore throat.
 Image courtesy of David Castillo Dominici at FreeDigitalPhotos.net
Image courtesy of David Castillo Dominici at FreeDigitalPhotos.net
An URTI is usually a self-limiting syndrome that typically resolves within 3 to 10 days. Symptomatic treatment remains the cornerstone in the management of viral URTIs. As antibiotics have no direct effect on viral infections, using antibiotics for viral infections is not recommended. Furthermore, the unnecessary use of antibiotics exposes patients to unnecessary risks of antibiotic side effects. At the same time, it contributes to the development of antibiotics resistance. Antibiotics are indicated only in the rare occasion that complications involving bacterial infections arise, for example when pneumonia is diagnosed.Majority of URTIs are caused by a virus, such as the Rhinovirus, Parainfluenza virus, Adenovirus and the most notorious Coronavirus. These viruses are the main culprits of the common cold, which is different from flu. Flu tends to be more severe and is caused by the Influenza virus.
Why should I go for flu vaccinations?
As the saying goes, prevention is better than cure. Annual flu vaccinations can greatly help to reduce the chances of getting URTIs, so try not to put it off! As the flu strains change from year to year, annual vaccination with the latest flu vaccines is recommended. Simple steps in personal hygiene can go a long way too! Practise good hygiene by coughing or sneezing into a tissue, keeping hand hygiene and putting on a mask, especially if you have a cold or flu! Always remember: “Protect your loved ones with good personal hygiene, starting today!”

